Training: Health Care Providers
When one or more items in an MTG Confirmation prior authorization request (PAR) is denied by the claim administrator at Level 2, the health care provider has the option to resubmit some or all of the denied items as an MTG Variance PAR. This will populate a new draft MTG Variance PAR instead of requiring the health care provider to re-enter all the data required to create the PAR. Any item that is converted to a Variance PAR can no longer be escalated for a Level 3 review by the Medical Director's Office (MDO) under the Confirmation PAR. The provider will have the ability to escalate to a Level 3 review with the MDO any items on the new Variance PAR that are denied for medical reasons, or granted in part.
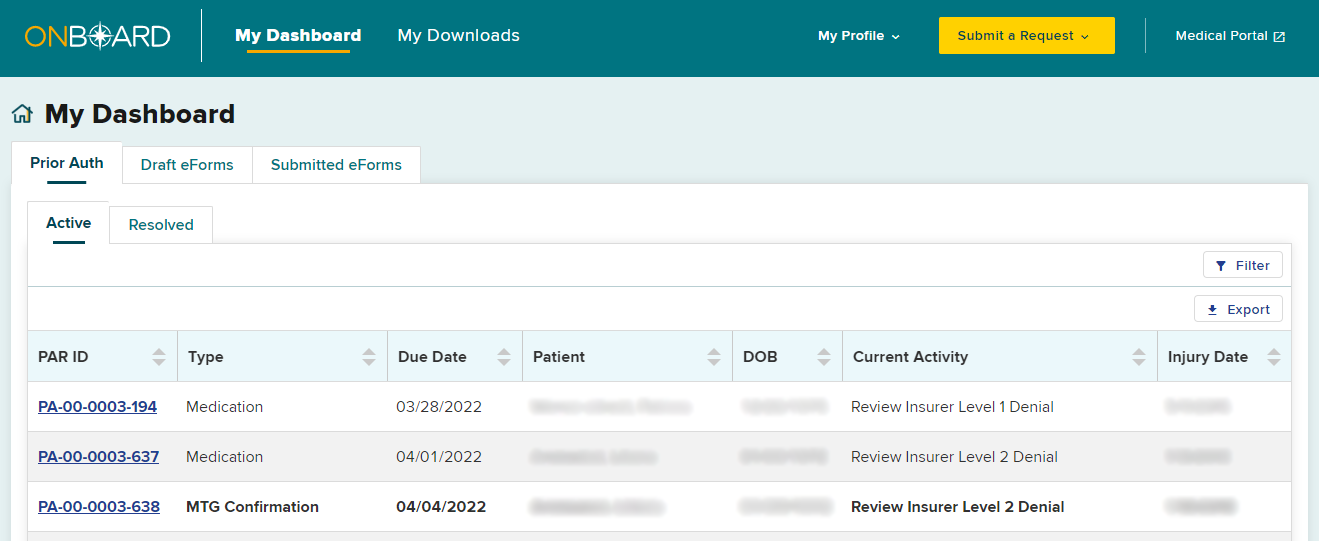
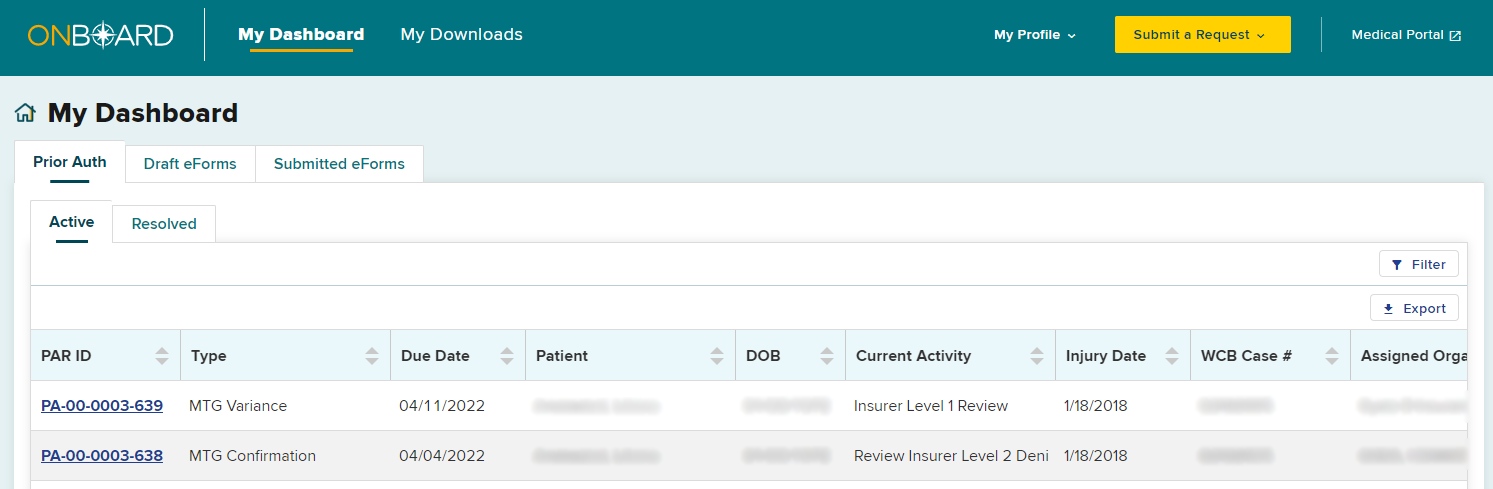
When an MTG Confirmation has been denied by the claim administrator’s Level 2 reviewer, the PAR row on the dashboard will change to bold. To convert the denied MTG Confirmation to an MTG Variance, select the PAR ID link.
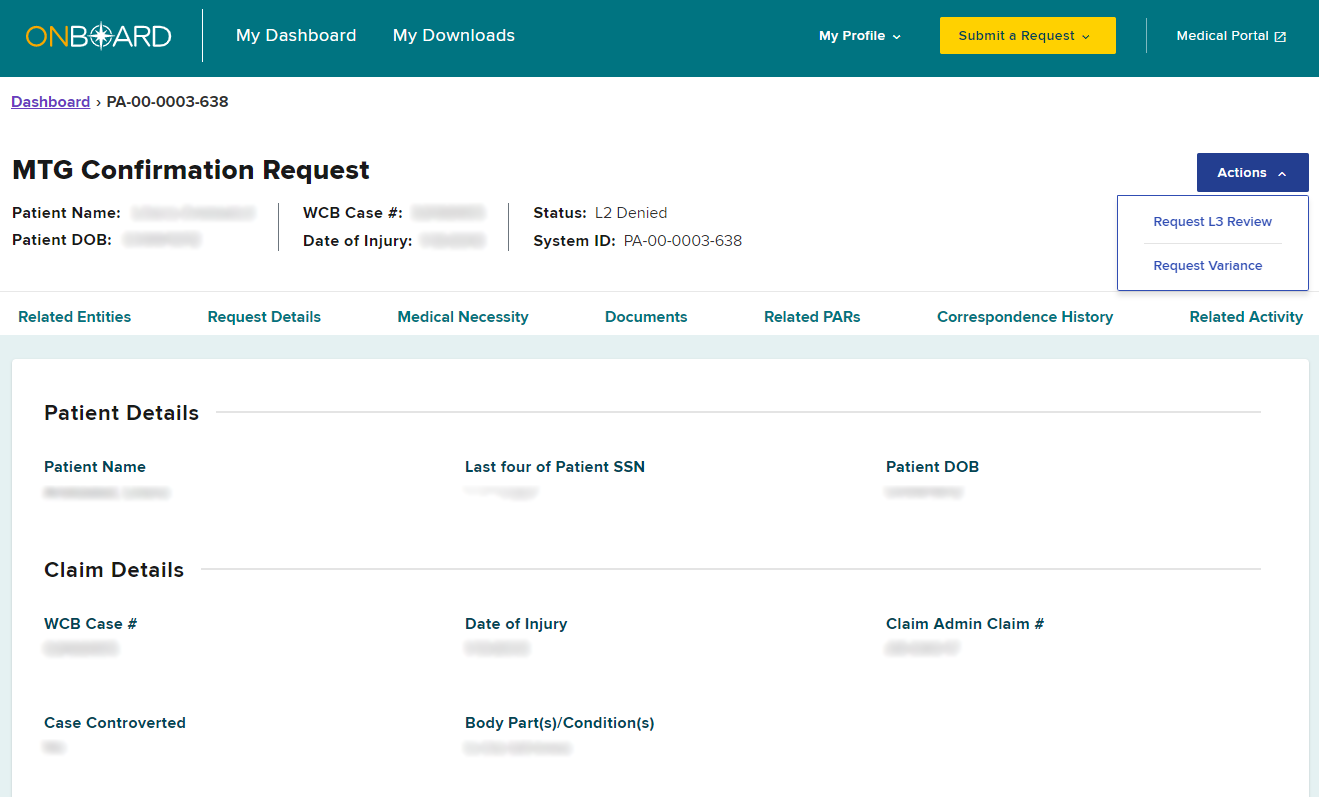
On the PAR Details page, select the Actions button on the top right and then select Request Variance.
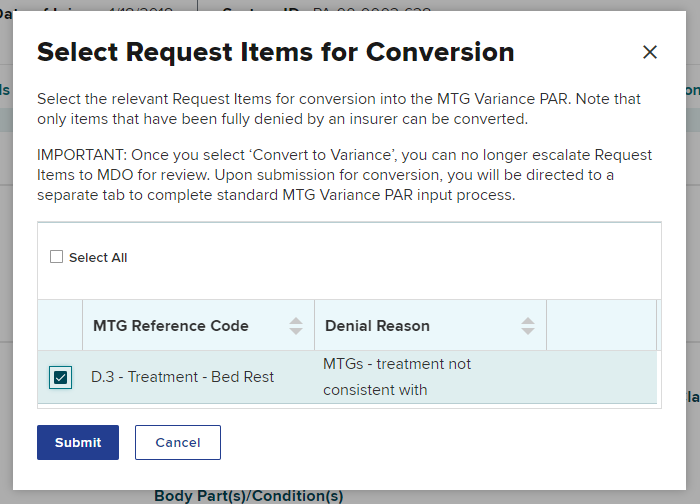
A pop-up will appear for you to select the MTG Confirmation PAR item(s) you want to change to an MTG Variance PAR. If more than one item was denied on the MTG Confirmation PAR, you can select specific items or select all then select Submit.
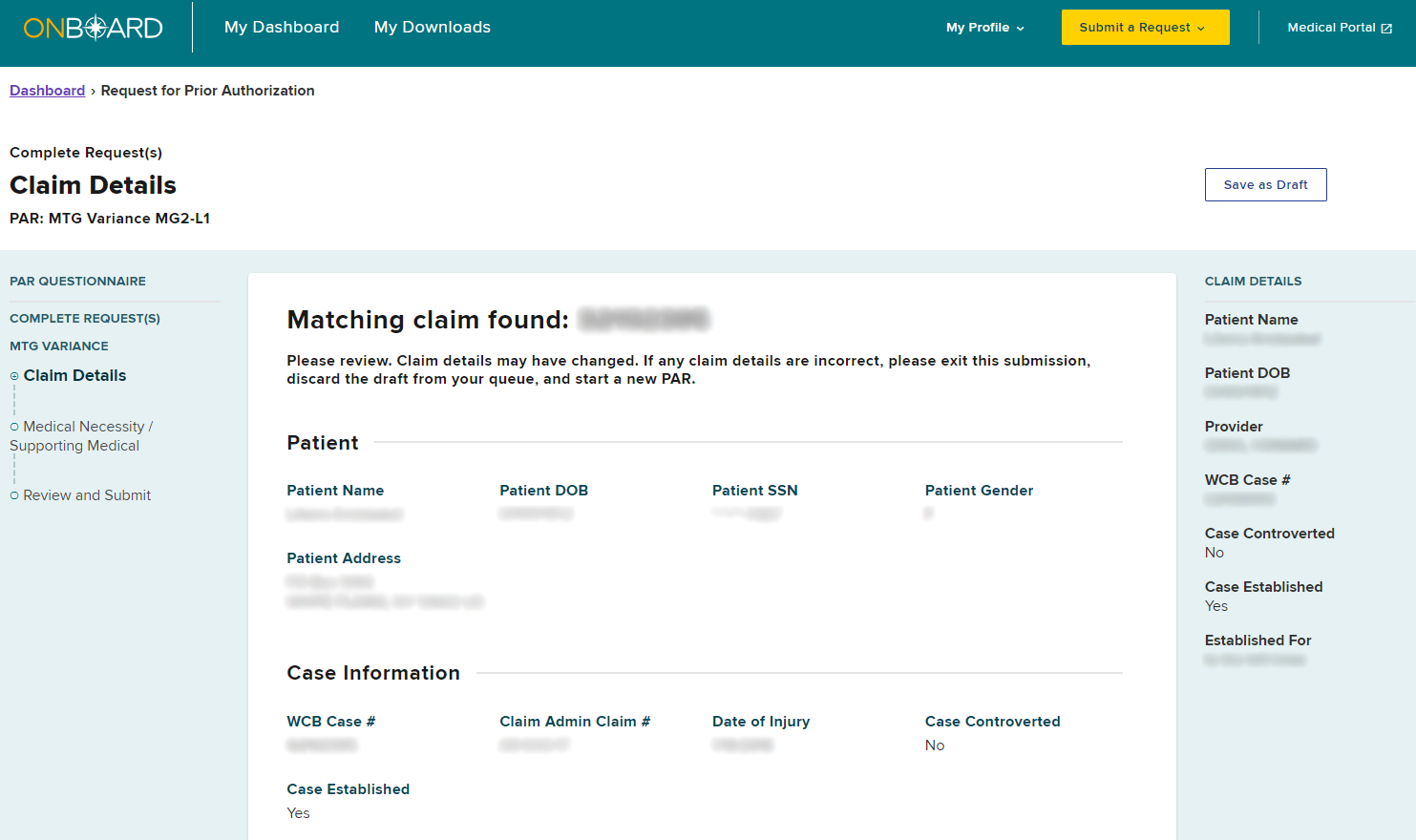
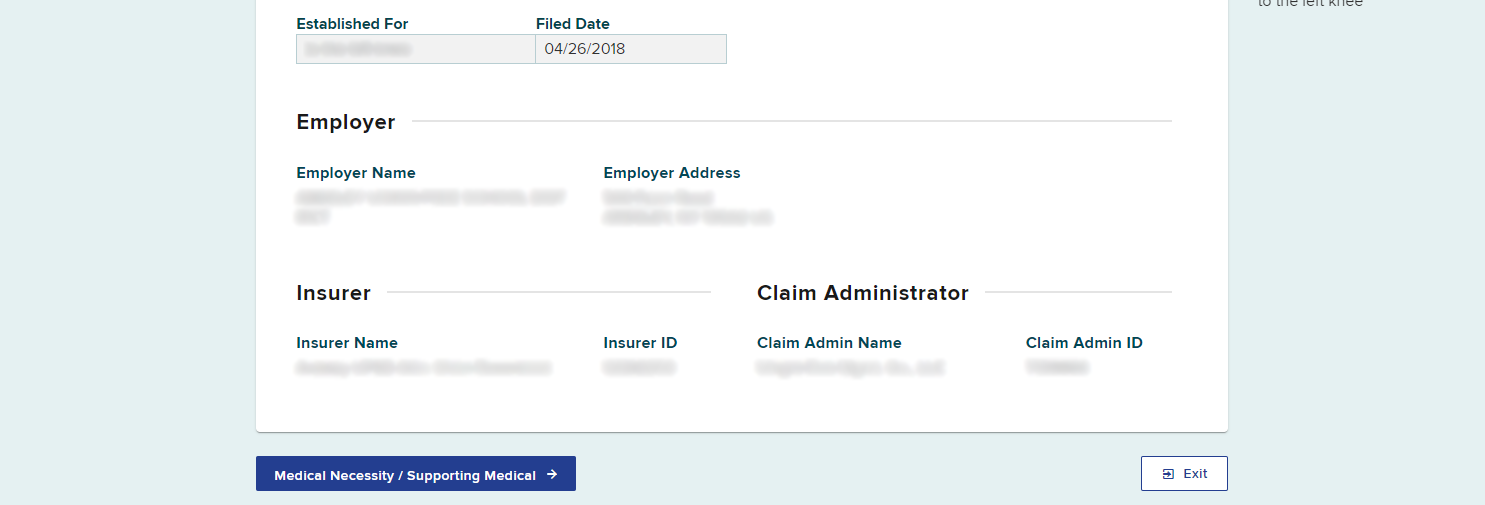
After selecting Submit, a new tab will open in your browser. This new tab will contain the new MTG Variance PAR. The claim details will be the same as the original MTG Confirmation. If details need to change, exit this submission and create a new PAR. To continue with the submission, select Medical Necessity / Supporting Documentation.
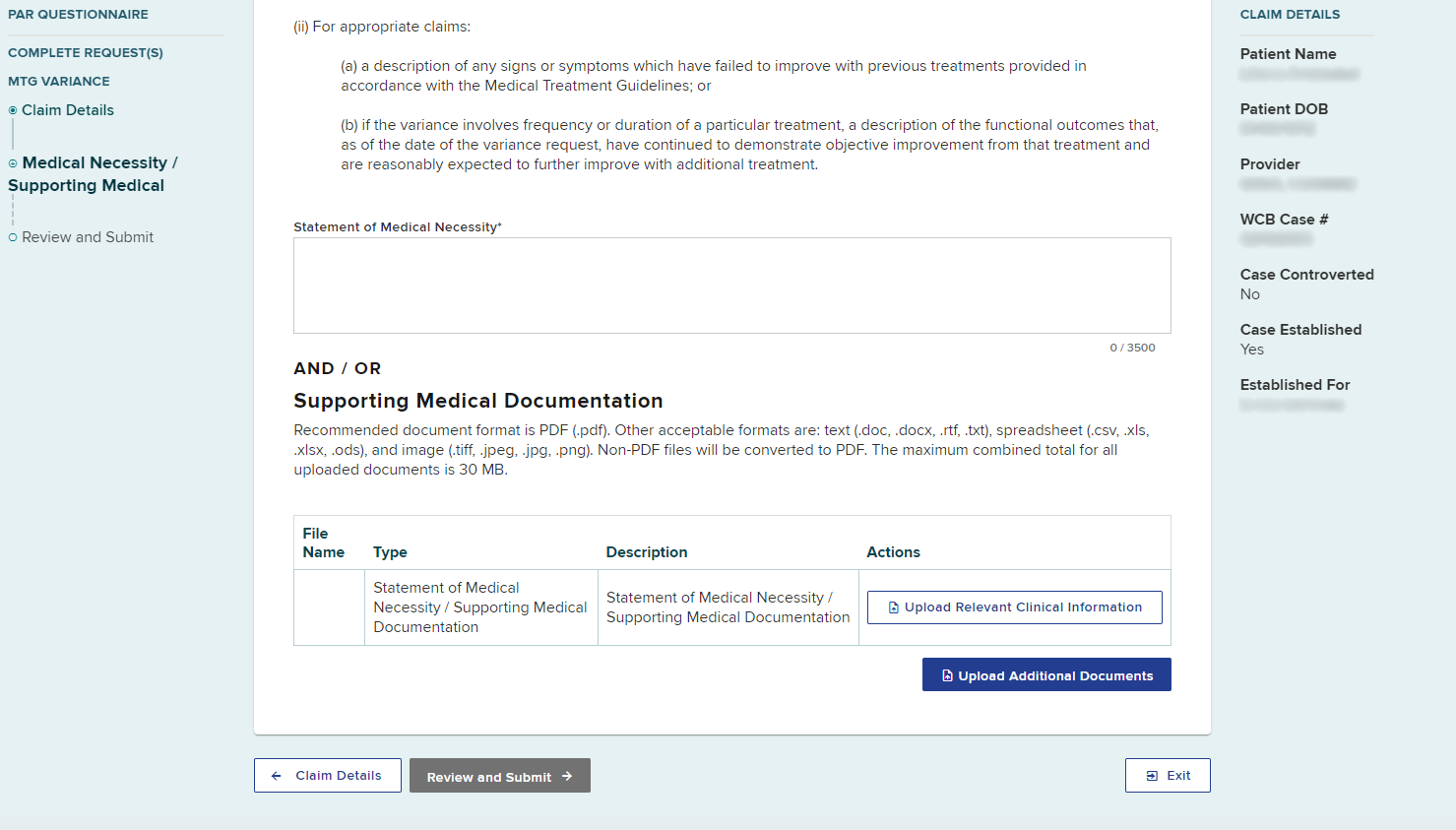
Enter or upload documentation that supports the MTG Variance request and then select Review and Submit.
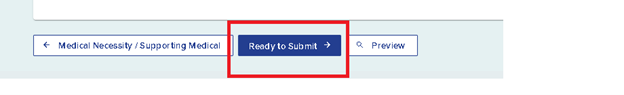
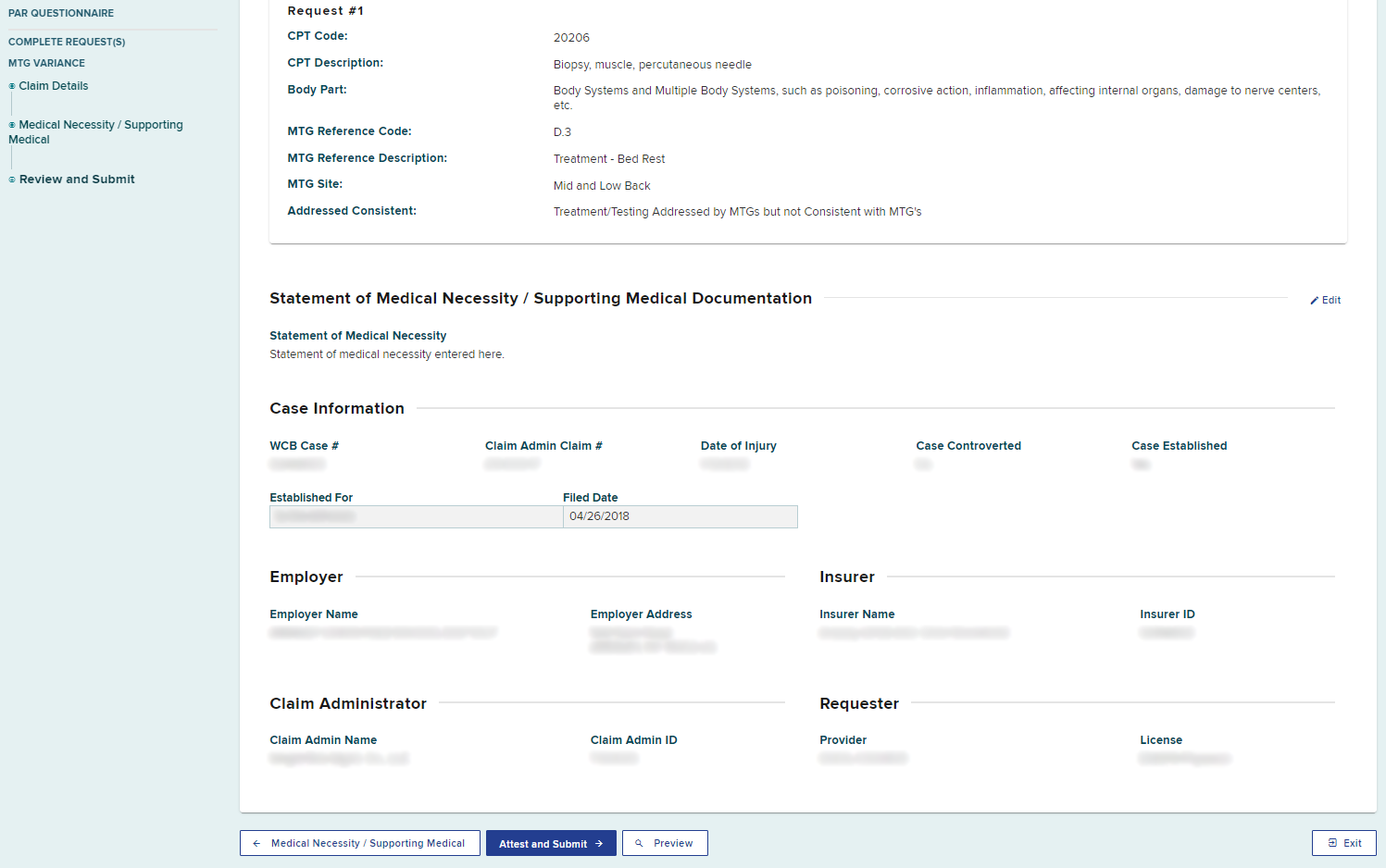
Review the details of the request. If you are the provider’s delegate, select the Ready to Submit button. This will add the PAR to the Draft eForms queue with a status of "ready to submit" for all delegated users and the health care provider. The health care provider must complete the process by signing and submitting the PAR. Drafted eForms will be automatically removed from the system after 30 days if they are not submitted.
If you are the provider, select the Attest and Submit button.
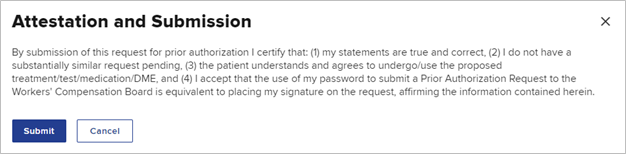
The provider is required to understand all aspects of the attestation presented to them before submitting a PAR. Select Submit to attest and submit the PAR.
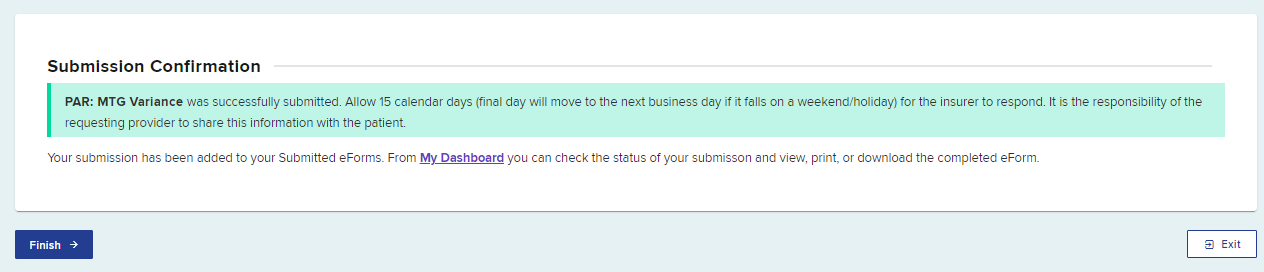
A confirmation page will show, confirming your PAR Variance submission, which includes the timeframe for an expected response.
Select Finish when done.
The new MTG Variance PAR will now show in your Submitted eForms tab.
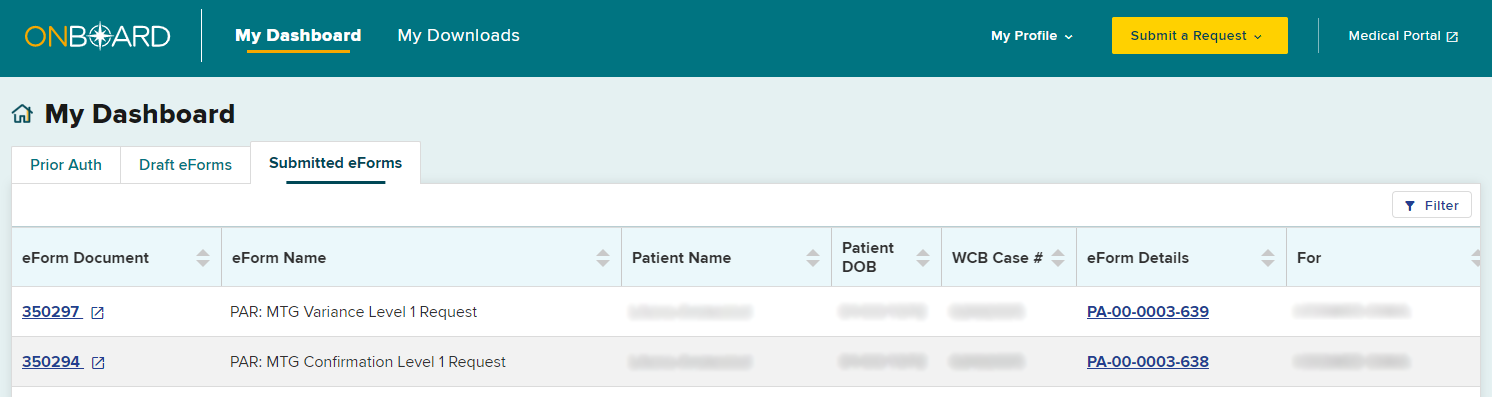
The Active tab in your dashboard will also update with the new MTG Variance.
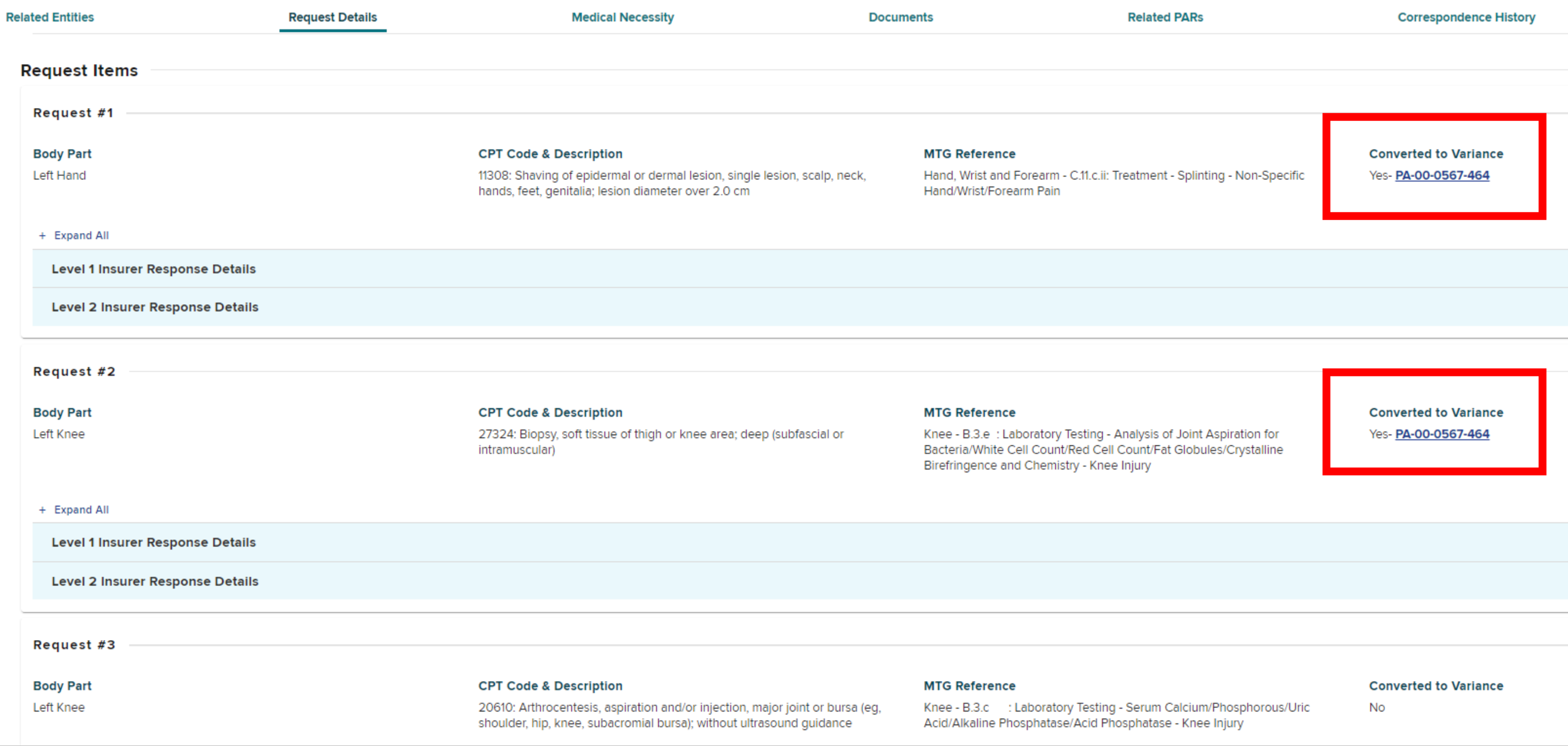
If a prior authorization request contains multiple request items and a provider has converted one or more MTG Confirmations to MTG Variances, those request items will show "Converted to Variance" as Yes and contain a link to the Variance request.