Update Claim Sender and Request Insurer Review
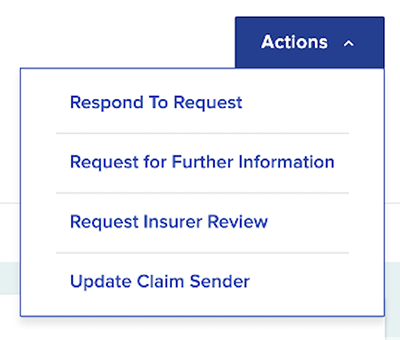
Payers have the option to update the claim sender or request insurer review of a PAR. These Actions options will be available on the PAR Object details page: Request Insurer Review and Update Claim Sender.
Requesting insurer review or updating the claim sender can only be done by the payer workload administrator when a PAR is in Level 1 review status, and each option can only be done once per PAR. This action cannot be completed by someone holding a Pharmacy Benefit Manager (PBM) or Medical Review Organization (MRO) workload administrator role.
Update Claim Sender
Updating the claim sender allows the workload administrators to reassign the claim administrator assigned to a PAR. For example, if a third-party administrator (TPA) takes over a claim, the previous TPA will have the ability to reassign a related PAR if it is routed to them.
To update the claim sender of a PAR, select Actions and Update Claim Sender when a PAR is opened.
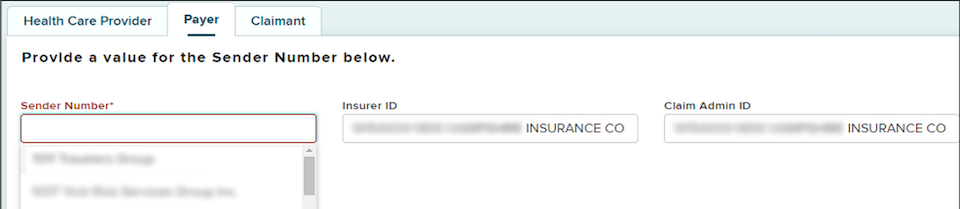
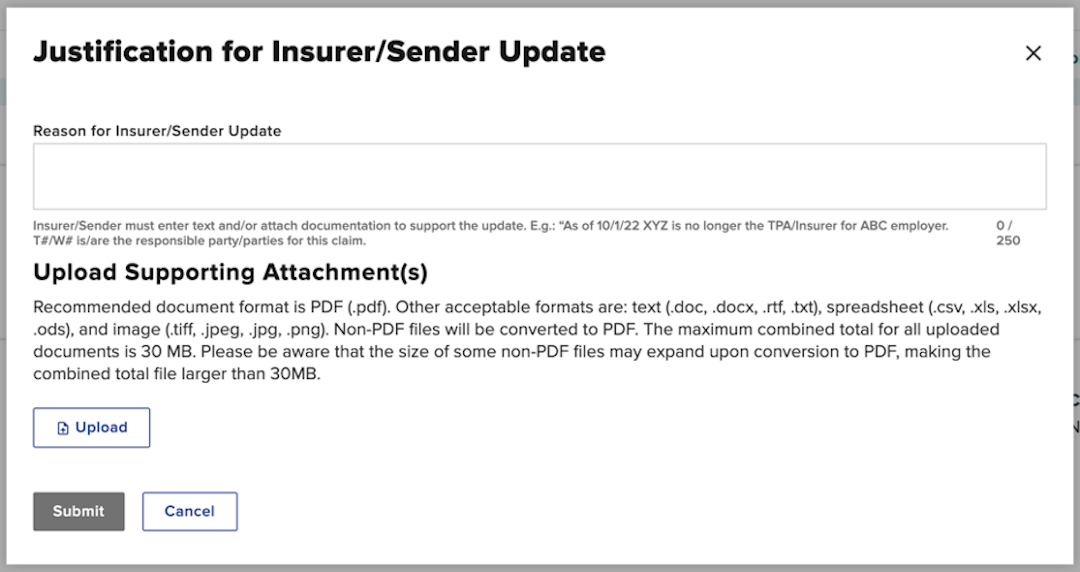
You will be redirected to the Justification for Insurer/Sender Update page. After the justification is submitted, the workload administrator will be redirected to the Payer tab and may update the Sender Number (claim administrator) and Claim Admin ID. The Insurer ID will be pre-populated from the PAR and cannot be edited.
After the workload administrator selects the new Sender Number and Claim Admin ID, the PAR is reprocessed, email notifications are sent, a new document is generated, and the PAR is routed to the correct sender.
Request Insurer Review
Workload administrators have the option to submit a request for insurer review on PARs they think have been sent to the incorrect insurance carrier. This should only be used if a payer does not have the ability to reassign the PAR to the correct claim administrator under the Update Claim Sender option.
To request insurer review, select Actions and Request Insurer Review.
When this is selected, a pop-up will display prompting the workload administrator to submit proof of the responsible entity via uploaded documents or free text entry in order to proceed.
Upon submission, the PAR status column temporarily updates with Pending - WCB Insurer Review and the proof is stored in the Documents section of the PAR details page.
If the Request Insurer Review submission is accepted, the Board will update the insurer information and the PAR will be routed to the new insurer for review. The PAR cannot be reassigned a second time.
If the Request Insurer Review submission is rejected by the Board, the workload administrator who submitted the request will receive an email notification indicating the request for insurer review has been rejected and the insurer is correct as assigned. The PAR will reset to an "L1 Requested" status for response.
PAR due dates are not extended if an insurer review is rejected by the Board. The Board suggests ensuring you are not the responsible claim administrator before requesting insurer review.