Overview
The Workers' Compensation Board has procedures in place to ensure that all parties get paid in a timely manner. If a payer has not paid a health care provider's bill, the provider may be able to request the Board's assistance by filing a Request for Decision on Unpaid Medical Bill(s) (Form HP-1.0) online, through the Board's business information system, OnBoard. On this page, we'll share instructions and requirements for submitting Form HP-1.0, and other important information for providers and payers on the medical billing arbitration process.
Request for Decision on Unpaid Medical Bill(s) (Form HP-1.0)
Payers are required to pay a health care provider's bill in full or submit a Notice of Objection to Payment of a Bill for Treatment Provided (Form C-8.1B) within 45 days of submission. If a payer has failed to do this, the health care provider may be able to request the Board's assistance by filing Form HP-1.0 through OnBoard. The Board's paper Form HP-1.0 is no longer being accepted. Payers are also responsible to pay the uncontested portion of bills within 45 days per 325-1.25(c) (2).
Note: Form HP-1.0 may not be submitted if less than 45 days have elapsed from the submission date of the bill or if the provider received a timely Form C-8.1B from the payer and the legal objection(s) related to the bill have not yet been resolved.
A few reminders:
Once a health care provider has received access to the Medical Portal, they should sign into OnBoard and select Submit a Request and then Form HP-1.0 to get started. The eForm will guide the provider step-by-step through the process of completing the request.
Required documentation
A complete medical bill must, by definition, include:
- a CMS-1500, and
- the supporting medical narrative.
When submitting a Request for Decision on Unpaid Medical Bill(s) (Form HP-1.0), providers must also attach:
- Basis for provider belief that the clinical intervention was medically necessary; AND
- Payer denial communications (if received); AND
- Scenario-specific documentation.
Below breaks down the specific examples of documentation required:
- Basis for provider belief that the clinical intervention was medically necessary
- If the clinical intervention at issue was consistent with the Workers' Compensation Board's New York Medical Treatment Guidelines (MTGs), please attach one of the following:
- MTG Confirmation prior authorization request (PAR) granting the clinical intervention, OR
- The summary page from the Board's MTG Look Up Tool, diagnosis, and clinical intervention in question. The MTG Lookup Tool can be accessed within the Medical Portal, OR
- A copy of the applicable section of the appropriate MTG indicating that clinical intervention was "recommended" pursuant to the MTGs, OR
- Alternatively, if the clinical intervention at issue varied from the MTGs, or otherwise required a PAR, please attach one of the following:
- A copy of the PAR granting the clinical intervention, OR
- A copy of any Order of the Chair and/or any Notice of Decision/Resolution granting the clinical intervention, OR
- Payer denial communication (if received)
- Scenario-specific documentation
Alternatively, certain services are not driven by the above and do not typically involve the submission of a PAR, but rather, the documentation will come from the various scenarios listed below. For example, emergent care and ambulance services do not typically require a PAR. Similarly, office visits with evaluation and management codes only and DME consistent with the MTGs and billed within the applicable fee schedules may not have PAR documentation, AND
If the provider has received from the payer a Notice to Health Care Provider and Claimant of an Insurer's Refusal to Pay All (or a portion) of a Medical Bill Due to Valuation Objection(s) (Form C-8.4), that should be submitted as well. If received by the provider, this should also include an Explanation of Benefit (EOB) communication from the payer, AND
The Board has outlined specific documentation that should be provided in support of the most common billing dispute scenarios (please see below), which should also be submitted with the Form HP-1.
Payer response
Upon receipt of a CMS-1500 form, payers have 45 days to respond. They can either pay the medical bill in full, or object by submitting a Notice to Health Care Provider and Claimant of an Insurer's Refusal to Pay All (or a portion) of a Medical Bill Due to Valuation Objection(s) (Form C-8.4), along with required documentation, to the Board and the health care provider. As described in the table below, payers are encouraged to submit an Explanation of Benefits (EOB) upon the submission of any valuation objections; failure to do so may result in an award in favor of the provider.
How the Board resolves the unpaid medical bill varies depending upon:
- Type of care provided
- Objection(s), if any, raised by the payer
Administrative award
- HP-1.0 forms submitted in instances wherein a Board-authorized provider did not receive a timely valuation objection to payment (Form C-8.4) or services provided in New York State.
- The Board creates an administrative award based on the New York State Workers' Compensation Fee Schedule.
- Payers may submit a written response for Board consideration.
- Based upon evidence provided by the payer, the Board will rescind or uphold the award.
Arbitration
- HP-1.0 forms submitted by a Board-authorized provider who received a timely valuation objection Form C-8.4.
- HP-1.0 forms submitted for treatment provided outside of New York State.
- HP-1.0 forms submitted by providers who are ineligible for Board authorization (e.g., Durable Medical Equipment supplier, pharmacy, out of state provider) regardless of valuation objection.
Arbitration process
To streamline and make the arbitration process more efficient for all parties, the Board has implemented the following procedures:
- Upon the receipt of a Request for Decision of Unpaid Medical Bills (Form HP-1.0), scheduling of an arbitration date, and issuance of a Notice of Arbitrator Review on Disputed Bill (Form HP-6R-D), the Board will provide notice to both parties to the arbitration, including detailed instructions as to how to submit materials and the recommended materials to support their respective positions in the arbitration.
- The parties will be given 30 days to respond to the information request so that the materials can be appropriately processed for and reviewed by the arbitrator in advance of the arbitration date. Materials received after the 30-day deadline may not be considered for review.
- Specifically, the parties will be asked to provide up to a 250-word rationale, describing their position in the pending arbitration.
- They will also be asked to provide up to 20 pages of documentation to support their position. Materials submitted in excess of 20 pages may not be reviewed, at the discretion of the Board.
- Specific recommendations for the types of information that should be submitted, based on the nature of the fee dispute, are provided in the Arbitration scenarios and recommended actions section.
- The parties will be asked to use Form HP-6R-D as a cover sheet for all submissions in support of their fee arbitration. This allows for easy identification and triaging of information and will not count against the party's 20-page limit.
- For arbitration scenarios not identified on the Arbitration scenarios section, please submit any relevant supporting documentation within the 250-word and/or 20-page restrictions.
- While submission of these materials is optional, please be advised that the arbitrator is permitted to consider a lack of documentation submitted in support of your position as an indication that such documentation may not exist.
- Submit supporting documentation directly to the Medical Director's Office as a PDF attachment to arbitration@wcb.ny.gov or via fax to 518-474-8898 only. Documentation submitted to other email addresses or fax numbers may not be reviewed.
Note: The Board will not accept any request for an administrative and/or arbitration award until 30 days after all issues timely raised by the payer/employer with respect to its legal liability for payment.
The best course of action is for documents to be submitted at the time a form is filed by a provider or payer. If the dispute is referred to arbitration, both parties will be asked to submit or resubmit their supporting documentation, but for those items referred for administrative awards, the only supporting documentation to be considered will be that which has already been submitted.
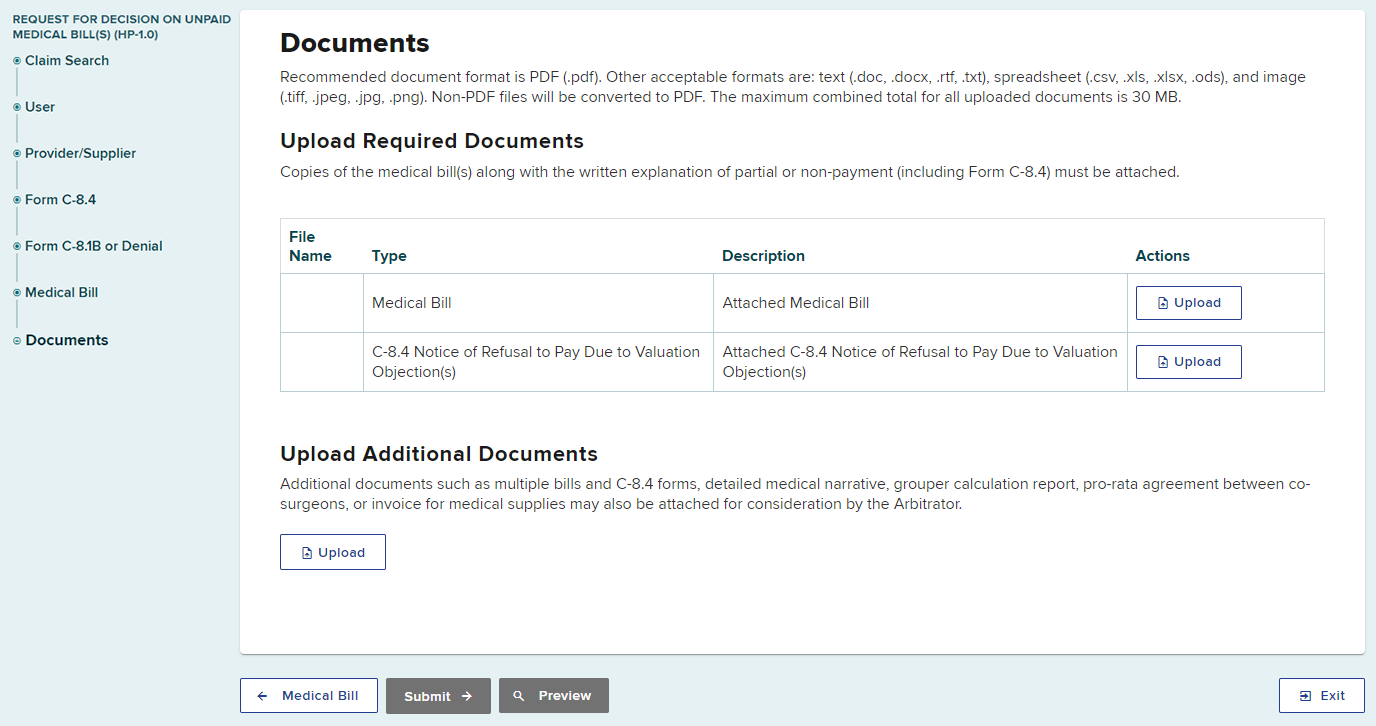
Below is a screen shot from the OnBoard training section of the Board's website demonstrating when and how to upload documents.
Arbitration scenarios & recommended actions
Below are common arbitration scenarios for payers and health care providers along with the recommended actions and supporting documentation each require. If you do not see your specific scenario, you may submit any relevant supporting documentation within the 250-word and/or 20-page restrictions as noted in steps 3 and 4 of the fee arbitration process, above.
| Payer scenarios | Action and/or documentation required |
|---|---|
| Billing in Excess of Allowable Daily Relative Value Unit | Please provide specific proof (e.g., check copies, cancelled checks, or other documentation that individual, provider-specific payment has been made, and not merely a listing of all provider bills from a particular date of service) that you have paid the other providers in this case for relevant and applicable services on the date of service in question. |
| Evaluation and Management Codes | If you have reduced payment, please explain, in 250 words or fewer, with specificity, why you reduced payment and provide a substitute CPT code for consideration by the arbitrator. |
| Frequency, Duration, or Number of Visits | If the issue is frequency, duration, or number of visits, please explain, in 250 words or fewer, with specificity, based on the Workers' Compensation Board's New York Medical Treatment Guidelines (MTGs), or best medical practices in those instances in which there are no MTGs, why the services should not be paid, or provide documentation that the services have already been performed and reimbursed. |
| Prior Authorization / MTGs | If the services require prior authorization and prior authorization was not granted, please submit any administrative or judicial communication from the Board indicating that the services were deemed not authorized. If the services require prior authorization and prior authorization was not requested, please provide any relevant references to the MTGs. |
| Preferred Provider Organization (PPO) Contract | The Board does not adjudicate, arbitrate, or otherwise referee billing disputes stemming from private contracts between providers and provider networks. Payers who knowingly apply fee reductions to providers who are not under a Preferred Provider Organization (PPO) contract are advised that this activity may be considered misconduct resulting in administrative action by the Board and that disputes may be awarded in the provider's favor per the New York State Workers' Compensation Fee Schedule (Fee Schedule) |
| Hospital Services or Facility Bills | In 250 words or fewer, with specificity, please provide a rationale for the total amount paid and the diagnosis related group (DRG) level paid for hospital services. |
| Payee (health care provider) scenarios | Action and/or documentation required |
|---|---|
| Withdrawal | If your disputed bill has been paid according to the Fee Schedule since you submitted your arbitration request, please submit a Notice to Chair: Health Provider's and Insurer's Withdrawal of Request for Arbitration (Form HP-4) to withdraw your arbitration request. |
| Prior Authorization / MTGs | If the services required prior authorization, please submit documentation indicating that the services were approved by the payer through OnBoard or via the appropriate administrative or judicial communication from the Board. In 250 words or fewer, with specificity, please explain the medical necessity for the services, and include the appropriate MTGs reference. If the services do not require prior authorization, please submit an MTGs Verification Summary from the MTG Lookup Tool demonstrating so. Documentation from the MTG Lookup Tool does not constitute a prior authorization nor does it constitute a guarantee of payment. |
| Evaluation and Management Codes | If the payer has reduced payment, please provide, in 250 words or fewer, with specificity, a rationale for the CPT code that you billed. |
| Frequency, Duration, or Number of Visits | If the issue is frequency, duration, or number of visits, please explain, in 250 words or fewer, with specificity, based on the MTGs, or best medical practices in those instances in which there are no MTGs, why the services should be paid. |
| Urine Drug Screens | Please provide a rationale for the frequency or type of drug testing performed, using specific references to the MTGs, the Fee Schedule, or both. |
| "By Report" Codes | For services designated as "by report" in the Fee Schedule, please provide documentation which meets the requirements of Ground Rule 10 of the Introduction and General Guidelines of the Fee Schedule. |
| PPO Contract | The Board does not adjudicate, arbitrate, or otherwise referee billing disputes stemming from private contracts between providers and provider networks. Providers participating in PPO networks who knowingly submit arbitration requests for amounts in dispute in excess of what is permitted by their PPO contracts may be subject to administrative action by the Board's Provider Compliance Unit. |
| Out-of-State Providers | If the disputed fee is based upon a specific fee schedule from another state wherein the doctor practices and injured worker resides, the provider should list the specific procedure code and calculation methodology. Failure to do so may result in an application of a lessor fee and/or non-reimbursement. If the patient lives in NYS and payment is made based on the fee schedule associated with the patient's NYS zip code, do not submit a Request for Decision on Unpaid Medical Bill(s) (Form HP-1.0) for additional reimbursement. |
| Hospital Services or Facility Bills | In 250 words or fewer, with specificity, please provide a rationale for the total amount charged and the DRG level billed for hospital services. You may also provide supporting documentation up to 20 pages. Documentation in excess of 20 pages may not be reviewed. Please include the discharge summary and any operative reports or notes. Please do not submit the entire hospital record. |
| Ambulatory Surgery Center | Include/attach the 3M calculation sheet/EAPG methodology billing with all HP-1.0 forms. Please submit copies of related approved prior authorization requests (PARs). |
| Administered Drugs | A failure to provide the following information may result in determination in favor of the payer:
|
| Imaging Services | Please provide us with a copy of a narrative report for the imaging service. |
| DME Vendors | Please provide an invoice for any miscellaneous code items showing price paid by the vendor. Please submit Form HP-1.0 for entire rental time frame and not for two-week individual rental periods. Submit one Form HP-1.0 for all durable medical equipment dispensed on a date of service. Please submit copies of related approved PARs. |
| Pharmacies | Please provide a copy of ordering provider's prescription, and any needed Formulary/PAR approvals. Submit supporting information from provider for non-customary dosage, quantity, or form. |
Provider's Request for Judgment of Award (Form HP-J1), Section 54-b, Enforcement on Failure to Pay Award or Judgment
If the payer fails to pay an administrative or arbitration award within 30 days after it is issued, health care providers may file Provider's Request for Judgment of Award (Form HP-J1) to request consent for judgment and a certified copy of the award. These documents must be filed with the appropriate county clerk's office within 30 days following their execution.
Please note, the interest rate on unpaid bills is 1.5% for each 30-day period after the bill has become due and payable and in which the bill has not been paid.
Note: To avoid the complications of filing unnecessary requests, waiting 60 days is recommended. The 60-day time-period will allow for payers' billing/payment cycles.
For more information on medical bill disputes, please call (800) 781-2362.
Payment for medical testimony
The Request for Decision on Unpaid Medical Bill(s) (Form HP-1.0) process is not appropriate for bills related to medical testimony. However, the Board may be able to assist health care providers who have not been paid for this service.
A medical witness is entitled to a witness fee pursuant to Part 301 of Title 12 of the Official Compilation of Codes, Rules and Regulations of the State of New York.
Within 10 days of the completion of a witness's deposition, the party responsible for such witness's fee, if any, pursuant to the Workers' Compensation Law and regulations, shall remit payment of the fee to the witness. The fee is to be awarded in like manner as a witness fee, awarded for attendance at a hearing, irrespective of the location where the deposition takes place (including telephone and video testimony).
If the witness believes that a fee in excess of that set in Part 301 is warranted, the witness must submit a request to the Board within 10 days of the deposition. The Board will review the request and issue a subsequent decision concerning whether an additional fee is warranted.
If the health care provider is not paid within 10 days of the completion of a deposition, the provider should send a letter to the payer stating so.
The letter should include:
- the workers' compensation case number,
- the date of the deposition, and
- a request for payment within 10 days of the letter.
If the payer does not make payment within 10 days after the letter, the health care provider should send correspondence, via hard copy or email, to the Board requesting assistance. In each correspondence, please be sure to include the following, or else the Board will be unable to take any action:
- A cover letter, addressed to the Workers' Compensation Board, laying out:
- the date(s) of the testimony given,
- the date(s) on which payment was sought, and
- a statement that the doctor still has not been paid.
- Copies of any demand letters sent to the payer informing the payer that payment is owed. At least one of these demand letters should have been sent to the payer after October 2018 and should specifically indicate that:
- testimony was given on a particular date or dates;
- there was a direction for payment within 10 days of the testimony, but payment still has not been made; and
- asking for payment within 10 days of the receipt of the letter.
Note: Providers should not include/attach any additional documents (e.g., the subpoena that prompted the deposition, a bill for the deposition in the format of a CMS-1500 form, etc.) to the letter, as this may interfere with the processing of the request.
Hard copy correspondence must be sent to the Board's centralized mailing address:
NYS Workers' Compensation Board
Centralized Mailing Address
P.O. Box 5205
Binghamton, NY 13902-5205
If correspondence is sent to the Board via email, please include a cover letter as an attachment to the email; if the cover letter is only in the body of the email, it will not be properly processed. Such correspondence should be sent to the Board at wcbclaimsfiling@wcb.ny.gov.
The Board will review the request and, if it is determined to be substantiated, issue an Administrative Determination directing payment of the standard witness fee. Please note that the Administrative Determination will not provide for any additional fees.
If the payer still has not made payment 30 days after the Administrative Determination, the health care provider may contact the Board by mail or email to request further action.
Finally, please note that if there are multiple claims for which a provider is seeking a decision to compel payment, the provider should ensure there is a separate correspondence for each claim, and that they are not all included in the same correspondence.
FAQs
-
Can a provider submit a Request for Decision on Unpaid Medical Bill(s) (Form HP-1.0) if the treatment sought was denied by the payer and/or the Board's Medical Director's Office via a prior authorization request (PAR) and/or Workers' Compensation Law judge or conciliator?
No; treatment that was denied via a PAR or adjudication/conciliation process is not the responsibility of the payer or self-insured to pay, and therefore should not be billed to either the payer or the patient.
Please note, submitting Form HP-1.0 in instances where treatment sought was previously denied via a Board decision and/or resolution may trigger administrative and/or disciplinary action by the Board. Additionally, billing a patient directly for services relating to an on-the-job injury is a violation of Section 13-f of the New York State Workers' Compensation Law and may result in disciplinary measures.
-
Are providers required to submit an Explanation of Benefits (EOB) upon submitting Form HP-1.0 for non-payment?
Providers are strongly encouraged to submit an EOB upon the submission of Form HP-1.0 for partial payment of a bill; failure to do so may result in the rejection of Form HP-1.0. The Board will only consider documentation submitted at the time of Form HP-1.0 submission and will not retrieve information from the case file in support of the claim.
-
Are payers required to submit EOBs upon responding to a Board-issued administrative and/or arbitration award?
Payers are strongly encouraged to submit an EOB upon responding to a Board-issued administrative and/or arbitration award; failure to do so may result in an award in favor of the provider. The Board will only consider documentation submitted at the time of the payer response to a Board-issued award and will not retrieve information from the case file in support of the claim.
-
Are payers required to submit EOBs upon objecting to a bill via Notice of Objection to a Payment of a Bill for Treatment Provided (Form C8.1B) and/or Notice to Health Care Provider and Claimant of an Insurer's Refusal to Pay All (or a portion of) a Medical Bill Due to Valuation Objection (s) (Form C8.4)?
Yes; effective November 1, 2021, the Board requires simultaneous filing of all objections to medical bills. The objections should be made on Form C-8.1B (legal objections) and/or Form C-8.4 (valuation objections) and should be sent to the Board at the same time, along with a copy of the EOB/EOR. Failure to do so may result in an invalid objection and/or award in favor of the provider.
-
What is the penalty for failure to attach an EOB/EOR to the Form C-8.1B and/or Form C-8.4?
The Board will not impose a monetary penalty; however, the Board may find the objection invalid. The payer would be liable for payment of the full amount billed up to the maximum amount established in the applicable medical fee schedule.
-
How are ambulatory surgery center bills paid?
Ambulatory surgery center bills are paid by 3M/EAPG methodology. Please refrain from using other methodologies, as those will not be considered.
Contact
If you have questions or need assistance, you can email the Medical Fee Schedules & Billing Unit at disputedmedicalbills@wcb.ny.gov or call (800) 781-2362.